Over the past two decades, most governments in Asia have made important strides in their efforts to achieve universal healthcare. Healthcare has been a focus of policy reforms in the region not only in low-middle income countries such as India and Indonesia, but equally in high-income economies of Singapore and South Korea.
These efforts have contributed to improving health outcomes, better access to health services, and importantly lowering out-of-pocket (OOP) spending on healthcare. OOP expenditure on healthcare—the amount that individuals have to pay (for which they are not reimbursed) in accessing health services—is a metric to measure financial protection that health systems offer. High OOP spending can reduce access to needed services, and in some cases pushes vulnerable households into poverty or force families to borrow or sell assets to pay for medical expenses. China and Singapore, for example, have reduced OOP spending on healthcare by more than 50 percent, and Thailand from 30 percent to less than 10 percent over the past two decades. India has made similar gains in reducing maternal mortality rates in line to meet United Nations Sustainable Development Goals by 2030.
Notwithstanding these advances, there are several challenges in sustaining universal healthcare: healthcare costs are rising rapidly, public health systems are overwhelmed, existing healthcare infrastructure is stretched, and medical supply chains are fragmented. Many of these issues were brought into sharper relief during the COVID-19 pandemic.
Former US President Donald Trump’s famous quip ‘nobody knew healthcare was so complicated’ echoes the frustration of governments across the world with healthcare reform. It entails governments navigating and managing challenges around:
- adequate resourcing,
- getting the policy design right,
- working within existing institutions.
- dealing with entrenched and competing interests; and
- implementing health reform.
Importantly, these challenges need to be addressed at the same time. This in turn requires a public actor to have a magisterial overview of the health system, and the appropriate tools to intervene and implement reforms in one of the most contested policy domains. It is for this reason that healthcare reforms are likened to shaping a balloon: you address a problem in one aspect of the health system, and it manifests in an another.
These challenges notwithstanding, I do not have a pessimistic outlook of realising universal healthcare in the region. There has been increasing policy attention towards the sector over the past decade, and the pandemic has reiterated the importance of strong and resilient health systems. There is recognition in contemporary policy debates that public health crises like the COVID-19 pandemic that stretch are health systems are unlikely to be one-off events, and countries with universal healthcare are better equipped to managing such crises. But realising universal healthcare is a complex policy task.
My central argument is that achieving and sustaining universal healthcare requires addressing these specific challenges, which in turn require distinct policy capacities.
Resourcing
The first policy struggle relates to adequately resourcing the sector in the context of diminished fiscal capacity, and how those resources are distributed across the sector. Realising universal healthcare requires levels of public spending to which very few governments have been able to commit. Public spending on healthcare in most of the low-middle income countries in the region (India, Indonesia, Philippines, and Vietnam for example) has hovered between 1-2 percent of GDP over the past two decades. Most of this spending is allocated to recurrent expenditures leaving limited room for investing in other priority areas such as public health or programs to manage infectious diseases. After decades of policy neglect or deliberate efforts to rely on markets in healthcare, most countries in the region have come to rely on the private sector to finance healthcare. Most of this private financing is without sufficient risk-pooling such as insurance programs and is paid for directly by households through out-of-pocket payments. In some instances, these have pernicious effects in the case of severe illnesses including pushing vulnerable families into poverty.
Overcoming this sustained reliance on private financing requires governments to ramp up public spending on healthcare and many in the region have: Singapore’s spending on healthcare has increased significantly over the past ten years. It now spends about six percent of GDP on healthcare, about half of which is publicly funded—a far cry from the meagre three percent in the early 2000s. China is another example. While total health expenditures have not changed drastically (about five percent of GDP), public spending on healthcare now accounts for about half—a dramatic increase from 20 percent in the early 2000s. Many other countries, however, find it challenging to meet their commitments. For instance, expanding India’s flagship universal coverage program for the 60 percent of the population currently not covered is fiscally tenuous. Similarly, while Indonesia has announced the removal differentiated subsidies that its members received, the program does not cover pharmaceuticals which are a key driver of out of pocket spending.
Further, the pandemic changed the distribution of public spending. Governments are rightly focused on shoring up their public health systems, and meeting vaccination and pandemic preparedness goals. A recent report by the World Bank highlights that in many low- and lower-middle income countries increased levels of public expenditure on healthcare, but are unlikely to continue in the face of diminished fiscal space and shallow economic growth.
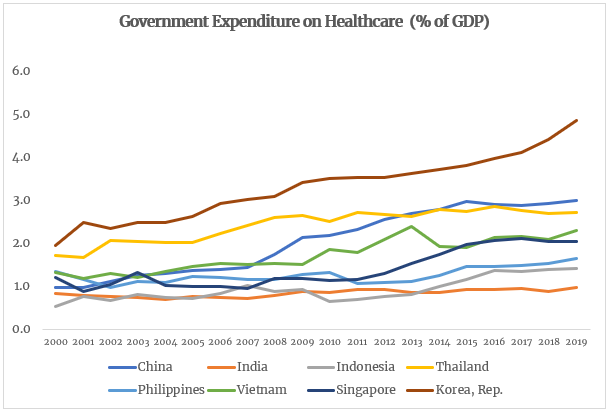
Source: World Development Indicators. Note: There is a three-year lag on comparable data on health expenditures.
Policy design
The second struggle relates to getting the ‘right’ design that underpins universal coverage programs. Essentially, realising universal coverage requires governments to achieve goals that are not easily reconciled. Governments are expected to design a healthcare system where citizens have universal access to medical services, and to ensure that healthcare providers remain responsive to patients’ needs at a cost that is affordable to the society. This is challenging, as different stakeholders prioritise these goals differently. Governments and third-party payers such as insurance companies are rightly concerned about moderating healthcare costs. Patients and providers prioritise responsiveness, immediacy of care and quality of care, but don’t want to shoulder the costs. These competing preferences are not easily reconciled.
For example, take the relatively straight forward issue of paying healthcare providers. Governments rely on a combination of Fee-For-Service (when providers are paid for each service they provide), Capitation (when providers receive a fixed amount per person they treat), Diagnostic-Related-Groups (when providers are paid a fixed amount based the patient’s symptoms and diagnosis), and Block Grants (lump-sum grants from the government) for different types of health services. Each of these offer fundamentally different incentives for controlling healthcare costs, and for being responsive to patients’ needs. Achieving both goals therefore require governments to use different types of payment tools to ensure that they work in concert.
This is again not easy to do—it requires access not only to disaggregated data on healthcare costs, demographic and epidemiological parameters, but the capacity to use this data and inform policy. This is an arduous policy ask not helped by limited resources. For example, Medicare in the US, which covers 40 million beneficiaries, is administered by a staff of 6,000 personnel with expertise in health administration. In contrast, the number of state-level personnel administering India’s health program is 42 in Uttar Pradesh, which has a population of 200 million, and 10 in Bihar, which has a population of 100 million.
International organisations such as the World Bank and the World Health Organisation have been instrumental in shoring up capacity, but there often remains a large gap between policy aspirations and actual policy practice. In the Philippines, for example, PhilHealth has been unable to fully implement its policy of ‘no balance billing’, where hospitals charge patients a nominal amount despite receiving subsidies. But all is not bleak on this front. Thailand’s investments in building research capability in its domestic health policy community in the early 2000s, has been central to adjusting the design of its flagship universal coverage scheme. India’s National Health Authority, the steward responsible for the government’s universal coverage program, has introduced a range of measures to collect and share data on costs and insurance claims.
The pandemic has not materially changed the design challenge around universal healthcare. It has, however, brought into sharper relief the need to invest in public health, and strengthen primary healthcare—an area not adequately prioritised in health policy reforms. Incorporating programs that prioritise these elements will require more design work for health policy agencies.
Institutions
A related issue is the constraints imposed by existing institutions in the sector. Institutions refer to formal organisations such as government agencies or private corporations involved in the sector, but also to established arrangements to organise healthcare such as Medisave in Singapore, PhilHealth in the Philippines, or the Employees State Insurance Corporation (ESIC) in India. These institutions are shaped by deeply held ideas and entrenched interests which constrain options available to policymakers when designing universal coverage programs.
For example, social insurance programs such as PhilHealth and Vietnam Social Security continue to exist despite extensive informal employment in their respective countries which makes these insurance programs poorly suited to achieving universal coverage. Similarly, the ESIC in India continues to exist despite a sustained track record of poor performance.
The lager point is that policy efforts to achieve universal coverage reforms have to navigate existing institutions that operate in the sector. These institutions have a certain inertia which often slows down reform efforts. Elections and even unexpected crises can temporarily lower these barriers and create an environment that is conducive to introducing new programs.
Efforts in India such as its universal healthcare plan Ayushman Bharath, or the Universal Coverage Scheme in Thailand are rare examples introduced after large electoral successes.
Most governments instead patch and layer existing programs, which creates challenges for policy coordination. For example, India’s 2008 health policy reforms resulted in a new program anchored in the Ministry of Labour rather than the Ministry of Health & Family Welfare raising issues for coordinating policy. The program was transferred to the health ministry in 2015.
Politics
The institutional impediments echo the political struggle of universal healthcare. This stems from asymmetric power relationships, an example of which is the dominance of healthcare providers such as hospitals and doctors’ groups in the healthcare system. The doctors’ role in diagnosing illness and prescribing treatment confers political power to providers which is used to resist any policy effort that erodes their material interests and undermines their professional autonomy. While they may compete individually for patients, they are bound together around the broader purpose of maintaining their material interests.
Universal coverage programs invariably involve changes to how healthcare providers are paid—moving them from retrospective payments (where providers are paid after treating patients, the most common example of which is fee for service) to prospective payments (where providers are paid a fixed amount such as salaries or capitation). Such efforts are typically resisted by providers and provider groups if they undermine their interests. Even governments with high political legitimacy, and publicly owned health systems such as in China, have found it challenging to introduce prospective payment reforms in the wake of opposition from provider groups
Providers are only one of the dominant stakeholders. Other groups such as labour unions and large insurance companies that underwrite health programs can stall reforms that undermine their interests. Raising resources for financing healthcare often through higher taxes or surcharges or asking citizens to pay more for accessing healthcare services are intertwined deeply with domestic politics about the distribution of scarce public resources. Overcoming resistance from interest groups, and engendering support across diverse and disparate stakeholder groups is central to the political struggle around universal healthcare.
Implementation
The final issue relates to the ongoing challenges associated with the operational aspects of universal healthcare. There are challenges around coordination, as well as working across different levels of government and across government agencies. Economics scholar Qian Jiwei in his analysis of health policy agencies in China estimates that there are at least 11 ministries actively involved in the delivery of services with overlapping responsibilities, which delays decision-making and creates multiple veto points. Similarly, a study published by the National Institute of Public Finance in India found that, in the state of Bihar, transferring funds from the federal agency to the state-level implementing agencies required clearance by 32 ‘desks’ which led to delays in the delivery of funds of almost 12 months. The sheer scale of universal coverage programs in India and Indonesia—about 250 million in Indonesia’s BPJS Kesehatan and 500 million in India’s Ayushman Bharath—present administrative hurdles to overcome exclusion and inclusion errors, especially in populations with large informal employment.
Another operational struggle for universal healthcare relates to the lack of robust health information systems and disaggregated demographic and epidemiological databases. These are central to generating data and evidence for the design of universal coverage programs. While there have been advances in developing these databases, progress has been patchy and uneven. For instance, in some states in India only 25 percent of deaths are registered in official records. The absence of such essential data reduces the efficacy of any social policy program.
Where to from here?
John Langenbrunner, a long-time observer of health reform in Asia at the World Bank, described policy efforts to achieve universal healthcare as a long march. Every country in the region is at a different stage of its journey. Yet, they face some common hurdles. In the high-income economies of Singapore and Hong Kong, recent policy efforts are focused on reducing long waiting times in their public systems. Their health systems have dealt with issues around controlling costs, improving quality of care, and the operational aspects of universal healthcare. Despite this success, they face pressures from elites and provider groups to increase levels of public spending.
Thailand, on the other hand, has achieved universal coverage with such low levels of spending that it faces the design struggle of improving the quality of care that the universal program offers. Its investments in building capacity of health policy agencies have helped develop and calibrate one of the most sophisticated payment systems among middle-income countries. The dominance of the Ministry of Public Health in financing and delivery of the system has helped address resistance to universal coverage reforms, and thus the program enjoys political support despite sustained periods of political instability and its political architect living in exile.
Vietnam and Philippines continue to deal with most of the struggles mentioned above. Despite concerted policy efforts over the past 10 years, governments have been unable to make meaningful inroads to reduce out-of-pocket payments. Part of this stems from challenges in the design—particularly how healthcare providers are paid—and in part the institutional inertia that Fee For Service payments enjoy, and a social insurance system that is poorly suited to realising universal coverage. Layered with this are operational challenges of enforcing existing regulations, holding errant providers accountable, and resistance from provider groups. Total health spending in both countries is relatively high compared to its level of economic development. Importantly, most of this spending is mediated through the private sector via out-of-pocket payments, reiterating the design struggle of universal health programs.
India and Indonesia’s universal coverage programs, the most recent in the region, reflect learning from health reforms in the region over the past 20 years. Their design relies on sophisticated prospective payment instruments, have reasonable levels of political support, and cohere with existing health policy institutions. The struggle in these countries is more on committing resources to scale the program and addressing operational impediments. Current public spending, less than two percent of GDP, offers limited instruments for the government to intervene in the sector and address its healthcare priorities.
Finally, there is the issue of trust in the health system. William Hsiao, a veteran observer of health reforms in low and low middle income countries, has maintained that the ultimate litmus test of universal health coverage is if the ordinary person has trust in the public health system. That is, is the public health system easily accessible, does it provide quality care, and importantly does it inspire confidence among citizens? During the pandemic, in many countries in the region, the public health system was the first point of contact in accessing medical services—the first interface with a system that has been neglected, underfunded, and resourced relatively to their private counterparts for decades. There is an urgent need to rebuild trust in the public health system among citizens and ensure that it not the last refuge of those who can’t access the private healthcare.
There is a tendency in contemporary policy discourse to conceptualise impediments to achieving universal healthcare as primarily fiscal in nature; that is, governments just don’t have the money to pay for universal healthcare. While this may be true in some instances, there are a range of other issues and challenges which public actors must navigate. Each of these struggles require fundamentally different sets of policy capabilities, and policy debates should focus more on developing these specific capacities to manage them if we are to make meaningful progress in realising universal healthcare.
Image: A child receiving a hearing test in India. Credit: Trinity Care Foundation/Flickr.